
However, the MRI can be normal in some cases, particularly with Type I FCD. In many cases of FCD, and particularly in Type II, the MRI is abnormal, showing an abnormally bright focal area on T2 and FLAIR sequences, which often has a characteristic “tail” extending to the margins of the ventricles. Epileptiform discharges are also commonly seen.
More suggestive of FCD is abnormal focal fast activity. The electroencephalogram (EEG) may show slowing of the background activity in the region of the FCD, however this finding is not specific for FCD and can be seen with other causes of epilepsy. In addition to seizures, FCD may result in clinical symptoms that result from focal disruption of brain function in the region affected by the dysplasia, such as language delays, weakness or visual concerns. The subtype of FCD correlates to some degree with age at onset, with FCD Type II presenting most commonly very early in childhood, and some cases of FCD type III presenting later in life. Less commonly, seizures can start in adulthood. FCD often causes seizures that onset in the first 5 years of life, and the majority will have seizures by the age of 16 years. The diagnosis of FCD can often be strongly suspected based on a detailed history and physical examination.

FCD Type I: the brain cells have abnormal organization in horizontal or vertical lines of the cortex.There are several types of FCD based on the particular microscopic appearance and associated other brain changes.
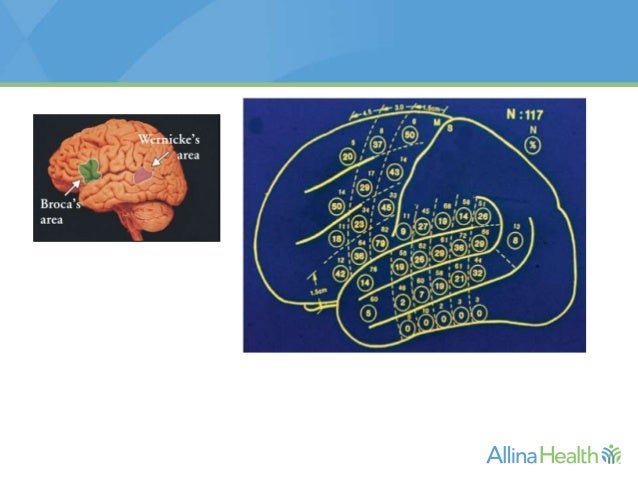
In FCD, there is disorganization of these cells in a specific brain area leading to much higher risk of seizures and possible disruption of brain function that is normally generated from this area.Brain cells, or “neurons” normally form into organized layers of cells to form the brain “cortex” which is the outermost part of the brain.Focal Cortical Dysplasia (FCD) is a term used to describe a focal area of abnormal brain cell (“neuron”) organization and development.


 0 kommentar(er)
0 kommentar(er)
